Erythropoietin (EPO): Benefits versus Risks
Erythropoietin versus Blood
Erythropoietin (EPO) is often presented as a medical breakthrough for treating anaemia and reducing blood transfusions. But not everyone agrees it’s the safest path. This article explores what EPO does, where it’s used, its known risks, and why My Medical Choice advocates for natural, ethical alternatives that support the body’s own healing instead.
Exploring a Common Blood Alternative
Erythropoietin, often shortened to EPO, is a hormone that plays a central role in red blood cell production. Since the 1980s, synthetic or “recombinant” EPO has been widely used in hospitals to treat anaemia, particularly among people with kidney disease, those undergoing chemotherapy, or patients preparing for surgery.
While EPO can reduce the need for donor blood transfusions, its use is not without controversy.
For an organisation such as My Medical Choice, which champions bodily autonomy, transparency, and ethical healthcare decisions, it is crucial that people understand both the pros and cons before consenting to such treatment.
This article aims to present a balanced and fully informed view, exploring the benefits, risks, and the philosophical considerations that guide MMC’s stance on EPO use.
What Is EPO and How Does It Work?
Erythropoietin is a naturally occurring hormone produced mainly by the kidneys. When oxygen levels in the blood fall, the kidneys release EPO to stimulate the bone marrow to produce more red blood cells (Jelkmann, 2011).
Synthetic EPO, also known as erythropoiesis-stimulating agents (ESAs), is manufactured through recombinant DNA technology, usually in genetically modified animal cell lines. The resulting hormone mimics the body’s natural EPO but is delivered as an injection, often weekly, to increase red cell counts in anaemic patients.
When Is EPO Prescribed?
1. Chronic Kidney Disease (CKD)
EPO deficiency is common in CKD because the kidneys lose their ability to produce the hormone naturally. Supplementing with synthetic EPO can improve haemoglobin levels and reduce anaemia symptoms (Locatelli et al., 2013).
2. Cancer and Chemotherapy
Chemotherapy can suppress bone marrow function, causing anaemia. EPO has been used to raise haemoglobin and reduce transfusion needs in these patients (Bohlius et al., 2009).
3. Pre-Surgical Blood Conservation
Before elective surgery, EPO may be prescribed to build a “personal blood reserve”, especially for patients who wish to avoid transfusions or where blood availability is limited (Muñoz et al., 2019).
In these contexts, EPO is often combined with iron supplementation to optimise red cell production.
How Effective Is EPO?
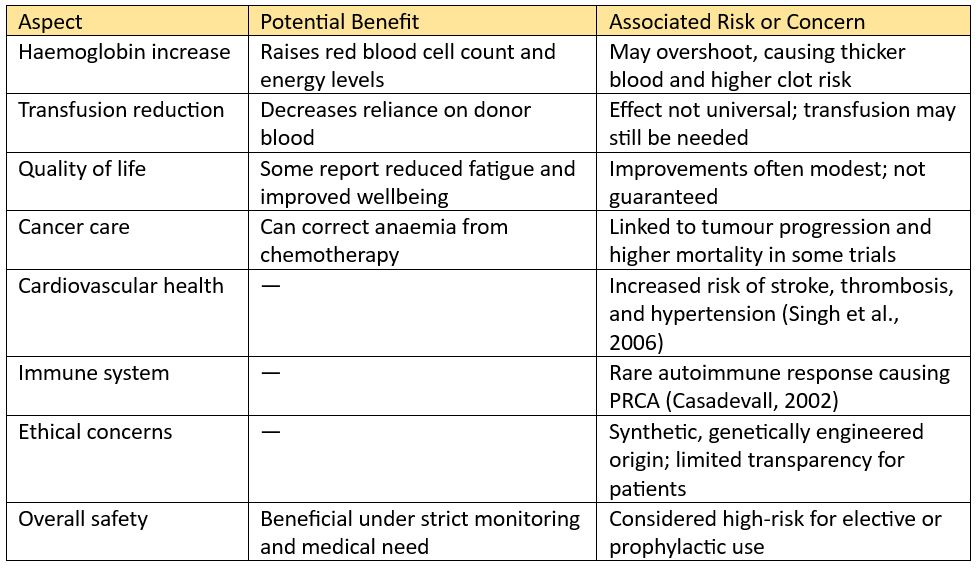
Clinical studies show that EPO can effectively raise haemoglobin and reduce transfusion requirements.
- In chronic kidney disease, up to 70–90% of patients respond with improved haemoglobin (Locatelli et al., 2013).
- In cancer-related anaemia, pooled trials show around a 36% reduction in transfusion needs compared with no EPO (Bohlius et al., 2009).
- In orthopaedic surgery, pre-operative EPO with iron has been found to lower transfusion rates and improve recovery haemoglobin levels (Li et al., 2016).
However, these figures focus narrowly on blood parameters and transfusion avoidance, not on long-term safety or overall patient wellbeing.

Known Risks and Safety Concerns
Although EPO is effective in increasing red blood cell counts, its risk profile has prompted growing caution in recent years.
1. Thrombosis and Cardiovascular Events
EPO can make blood thicker by raising its red cell content too quickly. Numerous studies link EPO use to an increased risk of blood clots, strokes, and heart attacks, particularly when haemoglobin levels exceed recommended limits (Singh et al., 2006).
The U.S. Food and Drug Administration and European Medicines Agency have both issued safety warnings advising strict haemoglobin targets to prevent these complications.
2. Tumour Growth in Cancer Patients
Some cancer cells possess EPO receptors, meaning the hormone can, in theory, promote tumour survival or growth. Evidence suggests that cancer patients receiving EPO may have higher mortality rates and faster tumour progression if used beyond specific criteria (Leyland-Jones et al., 2003; Bohlius et al., 2009). As a result, oncology guidelines now restrict EPO use to very defined cases.
3. Immune Reactions and Pure Red Cell Aplasia (PRCA)
Rarely, the body can develop antibodies that neutralise both synthetic and natural EPO, causing pure red cell aplasia, a severe condition where the bone marrow stops making red cells (Casadevall, 2002). Although uncommon, this complication can be life-threatening.
4. Other Side Effects
Commonly reported side effects include headaches, hypertension, joint pain, flu-like symptoms, and nausea. In some cases, patients have experienced seizures during rapid haemoglobin increases.
Summary of Benefits and Risks
Why My Medical Choice Does Not Endorse EPO
At My Medical Choice, our focus is always on helping people make well-informed, confident decisions about their healthcare. While EPO can raise red blood cell levels, it is still a synthetic, laboratory-made hormone that carries risks many people are unaware of. For those who prefer natural, low-risk ways to support their body, EPO may not feel like the right fit.
Our view is that genuine health should be strengthened through natural restoration and ethical medical care, not forced through artificial stimulation. The points below explain why we believe caution is both reasonable and responsible when it comes to EPO.
1. Respect for Natural Physiology
MMC’s guiding philosophy is to work with the body, not override it. EPO artificially accelerates red cell production rather than addressing why anaemia exists in the first place, which may stem from nutritional deficiencies, poor oxygenation, chronic inflammation, or organ dysfunction.
MMC therefore encourages approaches such as optimising iron, vitamin B12, folate, and oxygen therapy, which support healthy blood building naturally.
2. Avoiding Pharmaceutical Dependency
EPO is not curative; it must be administered repeatedly, often indefinitely in chronic cases. This creates dependency on pharmaceutical supply chains and ongoing clinical monitoring. MMC promotes self-empowerment and long-term autonomy rather than dependence on synthetic interventions.
3. Ethical and Genetic Concerns
Recombinant EPO is manufactured using genetically modified animal cell lines, typically Chinese hamster ovary (CHO) cells. For those who value clean, ethical medicine, this method of production raises both scientific and moral questions.
4. The Safety Balance
Even when EPO works, the margin between therapeutic and harmful is narrow. The potential for serious side effects, blood clots, heart strain, or tumour progression, makes EPO a questionable choice for otherwise stable patients seeking to avoid transfusions.
5. Informed Consent Above All
MMC’s mission is not to make medical choices for people, but to ensure every person has the right and information to decide for themselves. For many, this includes declining synthetic or genetically modified pharmaceuticals in favour of safer, natural alternatives.
A Natural Alternative: The National Blood Donor Database
To support members who wish to avoid both blood transfusions and pharmaceutical stimulants like EPO, MMC created the National Blood Donor Database, a practical, ethical, and transparent solution for those concerned about blood quality and medical autonomy.
The database helps people identify like-minded, compatible donors should surgery ever require a transfusion. Members are encouraged to form trusted arrangements with donors who have not received mRNA-based medications or therapeutics, and to document these relationships through a mutual-trust contract supplied by MMC.
To maintain harmony with the NHS, MMC advises donors also to register with the Red Cross or similar systems to confirm blood type and meet standard health requirements. Doing so ensures compatibility testing and cross-matching can take place if needed.
Members are encouraged to begin this process early. Building a donor list in advance provides:
- Peace of mind, knowing trusted support is in place.
- Mutual benefit, since donors and recipients can help each other.
- Community connection, linking people who share medical and ethical values.
MMC reminds all participants to proceed cautiously when contacting new donors, as all arrangements are private and voluntary. While most members will never need to use their donor network, simply knowing it exists can be profoundly reassuring.
In Conclusion
Erythropoietin has an established role in medicine, particularly where anaemia is severe or transfusions are unavoidable. Yet for those prioritising natural health, transparency, and low-risk care, it represents a complex ethical and physiological trade-off.
The evidence shows that while EPO can raise haemoglobin and reduce transfusion demand, it also carries measurable risks, including cardiovascular complications, tumour progression, and immune reactions. For My Medical Choice, those risks, combined with its synthetic origin, make it incompatible with a truly natural and autonomous approach to care.
Instead, MMC advocates informed preparation, building health through nutrition, natural blood optimisation, and ethical donor planning, ensuring that every individual retains ownership of their medical decisions.
Further Reading
- Bohlius, J., et al. (2009). Recombinant human erythropoiesis-stimulating agents and mortality in patients with cancer: A meta-analysis of randomised trials. The Lancet, 373(9674), 1532–1542. https://doi.org/10.1016/S0140-6736(09)60502-X
Comprehensive meta-analysis detailing EPO’s risks and benefits in cancer patients. - Casadevall, N. (2002). Pure red-cell aplasia and anti-erythropoietin antibodies in patients treated with epoetin. New England Journal of Medicine, 346(7), 469–475.
Seminal paper describing immune complications caused by EPO therapy. - Jelkmann, W. (2011). Regulation of erythropoietin production. Journal of Physiology, 589(Pt 6), 1251–1258.
Explains the body’s natural regulation of EPO and oxygen sensing. - Leyland-Jones, B. (2003). Breast cancer trial with erythropoietin terminated unexpectedly. The Lancet Oncology, 4(8), 459–460.
Reports tumour progression concerns in EPO use for cancer treatment. - Li, G., et al. (2016). The effectiveness and safety of preoperative erythropoietin in total hip or knee arthroplasty: A meta-analysis of RCTs. Journal of Orthopaedic Surgery and Research, 11(1), 25.
Shows short-term benefits of EPO in surgery but calls for caution in patient selection. - Locatelli, F., et al. (2013). Erythropoiesis-stimulating agents in chronic kidney disease: Current clinical practice. Nephrology Dialysis Transplantation, 28(6), 1346–1359.
Overview of EPO’s use and monitoring in kidney disease. - Muñoz, M., et al. (2019). International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia, 74(10), 1375–1389.
Supports pre-surgical blood optimisation through iron and conservative strategies. - Singh, A. K., et al. (2006). Correction of anemia with epoetin alfa in chronic kidney disease. New England Journal of Medicine, 355(20), 2085–2098.
Influential trial highlighting cardiovascular risks of aggressive EPO correction.
Is artificial blood the future of emergency medicine, or just another experimental promise?
Just a friendly reminder that no information in this publication constitutes legal or medical advice from My Medical Choice or any of our affiliates and the contents of this document are for educational and support purposes only.