Supporting Patients Choice Through Clearer Healthcare Planning
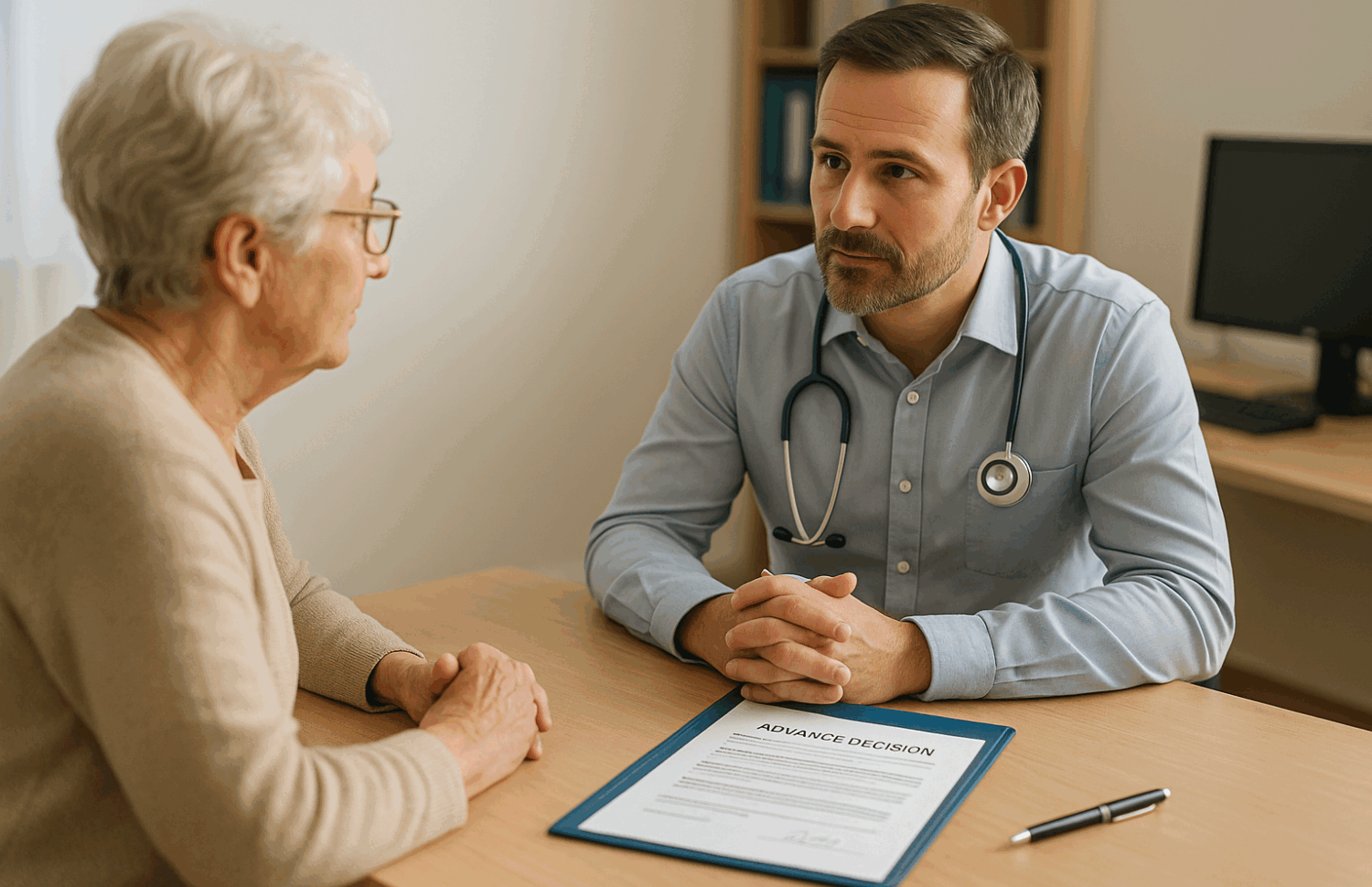
Advance Care Planning: Respecting Wishes in Times of Uncertainty
General practice has always been about relationships as much as treatments. Yet, continuity, the ability for patients to see the same GP regularly, is slipping away. This article explores why continuity is declining, why patients still value it so highly, and how personalised planning tools such as Advance Decision Notices can help preserve patient choice when it matters most. Drawing on recent studies and practical examples, it also looks at what this means for GPs today, and how proactive planning can strengthen trust, reduce pressure, and support care in emergencies.
Why continuity in general practice is slipping
In recent years, it has become noticeably harder for patients to see the same GP consistently. A major study in Annals of Family Medicine shows relational continuity fell from 29% in 2018 to just 19% in 2022, with broader variation among practices, highlighting growing unpredictability in care – {source}
Although access remains an issue, it’s vital to remember that continuity brings real benefits. Seeing the same GP consistently has been linked with lower emergency admissions, better long-term outcomes, and stronger patient trust – {source}
What patients are saying, and showing they value continuity
A 10-country survey involving UK adults aged 65 and over revealed concerning results: only 72% had a usual GP, compared with over 95% in countries like France and Germany. Continuity drops as staffing gets stretched. Seeing the same GP, however, has proven to reduce hospital admissions by more than 25% – {source}
In addition, a Cambridge study of 10 million appointments found that continuity extends the time between appointments by 18%, all while reducing future visit demand by about 5%. That’s equivalent to bolstering the GP workforce, and all without hiring new staff – {source}
What this means in everyday practice
Continuity isn’t just about convenience; it can make care safer and smoother. Take Mrs Ahmed, a 78-year-old managing three long-term conditions: with her familiar GP, problems are spotted early, fears are listened to, and plans are adjusted in context, not just treated in isolation. When continuity falters, clinicians risk missing subtle changes in health or values, leading to less thoughtful, more reactive care.
Care planning that truly matters beyond the form-filling
As the NHS pushes for personalised care plans by 2027, there’s a real risk they will become bureaucratic. This is where tools like Advance Decision Notices (ADNs) come in, they let patients record, in writing, the treatments they would refuse under certain circumstances.
That’s not about limiting medical care, it’s about supporting elected care that aligns with individual values, even when patients can’t speak for themselves. Advance care planning has been shown to reduce stress for families, improve end-of-life care, and enable clinicians to make informed decisions with confidence in complex situations.
Continuity in a changing system, still possible, still vital
The NHS is shifting toward larger, integrated structures, including ICPs, networks, and multidisciplinary teams, all of which are increasing the distance between patients and familiar faces. Yet, documented patient preferences, including ADNs and tools such as ReSPECT forms, help anchor patient values across various settings. ReSPECT, used in England to plan emergency and critical care, encourages conversations around what matters most, ensuring people are treated as people, not just cases.
Behind the scenes, practices that invest in relational and informational continuity—training reception staff to route requests to known clinicians, logging consistent preferences in records- are already mitigating fragmentation effects. One clinic that used EMR reminders to schedule follow-up with the same GP saw a real lift in continuity rates – {source}, and {source}
How My Medical Choice helps with advanced care
At My Medical Choice, we focus on making sure a person’s voice is not lost in an emergency. When decisions need to be made quickly, doctors and families can be certain of what the patient wants.
We support people in three key ways:
- Advance Decision Notices (ADNs): Giving legal weight to the treatments a patient wishes to refuse if they lose capacity – {source}
- Emergency Clarity: Ensuring that in urgent situations, clinicians have immediate access to documented choices, avoiding delays and uncertainty.
- Support for Families and Clinicians: Reducing stress at the bedside by making preferences clear, so care can continue with confidence and respect.
This approach doesn’t replace clinical judgement; it strengthens it by providing the information needed to act decisively and compassionately under pressure.
Dr Tina Peers discussing how being prepared gives her patients peace of mind
*Click on image, or follow –> {link}
Why this matters now
General practice capacity is strapped, but patients are still telling us what they value most: familiarity, being known, and autonomy. At a time when care models are shifting fast, embedding patient choice through clear documentation isn’t just a nice addition; it’s essential, practical, and humane.
Glossary of Key Terms
- Continuity of Care: The ongoing relationship between a patient and their GP, where the same doctor sees the patient regularly over time. This builds trust, avoids repeating histories, and often improves outcomes.
- Advance Decision Notice (ADN): A legally recognised document (under the Mental Capacity Act 2005) where a person sets out the medical treatments they would refuse in the future, should they lose the ability to decide or communicate.
- Advance Care Planning: A process where people think about and share their wishes for future medical care, so their preferences can guide decisions if they can’t speak for themselves.
- ReSPECT Process (Recommended Summary Plan for Emergency Care and Treatment): A UK-wide initiative where patients record their care and treatment preferences for emergencies. It focuses on “what matters most” to the person, not just on medical treatments.
- Integrated Care Systems (ICSs): Partnerships between NHS organisations, local councils, and other groups to plan and deliver joined-up health and care services in a region.
- Relational Continuity: Being cared for by the same GP or healthcare professional, creating familiarity and trust.
- Informational Continuity: Ensuring patient information (such as medical history, test results, and preferences) is consistently available to all clinicians involved in care.
- Management Continuity: Consistent and coordinated care plans across different providers and appointments, avoiding fragmented treatment.
When an Advance Decision Is Overlooked: A Wake-Up Call for Us All
Just a friendly reminder that no information in this publication constitutes legal or medical advice from My Medical Choice or any of our affiliates and the contents of this document are for educational and support purposes only.
