Assisted Dying Bill 2025: Safeguarding the Vulnerable Amidst Legislative Change
What is the End of Life Bill?
The Terminally Ill Adults (End of Life) Bill, commonly referred to as the Assisted Dying Bill, is currently under parliamentary scrutiny in the UK. While it aims to provide terminally ill adults with the option to end their lives with medical assistance, it has sparked significant debate regarding the adequacy of safeguards, particularly for vulnerable groups such as the elderly, disabled, and those with mental health conditions.
Medical Professionals Warn of Unexpected Risks
Several prominent doctors and medical organisations have voiced serious concerns about the Assisted Dying Bill, warning it may put patients and the medical profession at risk.
Risk to palliative care
Dr M W M Upton, a consultant neuropsychiatrist, cautioned in The Times that doctors might hesitate to prescribe vital medications like morphine if legal scrutiny over assisted dying intensifies. He fears palliative treatment could be delayed, prolonging patient suffering. {Link}
Vulnerability and coercion
A letter signed by more than 1,000 doctors, as reported by Sky News, stressed that the Bill “doesn’t protect patients, families and the medical workforce.” They raised particular concern that elderly patients, domestic abuse survivors, and financially insecure individuals could feel pressured into choosing assisted death. {Link}
Inadequate safeguards
These doctors warned that doctors get prognoses wrong about 40% of the time, meaning patients could unwittingly end their lives earlier than planned. The letter also points out that while assisted dying is enshrined as a right, equivalent access to comprehensive palliative care isn’t guaranteed.
Ethical and workforce threat
The Telegraph reported that doctors told MPs the Bill poses a “real threat to both patients and the medical workforce,” urging reassessment due to insufficient protections.
Pressure on mental health resources
A Times article echoed similar worries from top psychiatrists, who said that assisted dying could undermine broader suicide-prevention efforts, particularly among isolated elderly patients, and that mental health support within the Bill is inadequate.
Lack of oversight mechanisms
A Financial Times letter emphasised that the Bill removes independent judicial oversight, replacing it with panels that lack transparency. This, along with concerns from advocacy groups and psychiatrists, highlights the need for stronger protections to safeguard vulnerable individuals.
At My Medical Choice, our mission is to ensure that our members are fully informed and protected. We are closely monitoring the progression of this bill and are prepared to implement necessary measures to uphold our members’ rights and wishes.
Where we’re at as of 25/06/2025
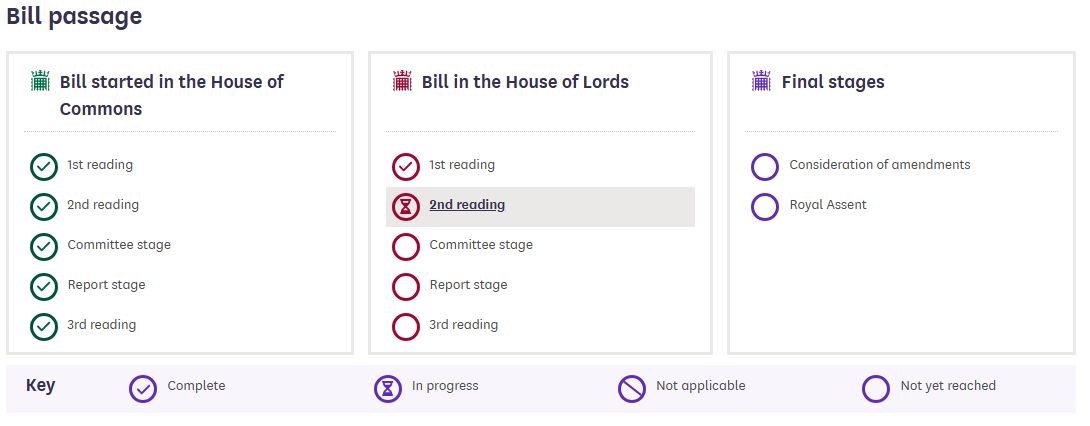
This graphic provides a clear overview of the current progress of the Assisted Dying Bill through Parliament as of June 25, 2025. It outlines the key stages the bill has passed, including significant votes in the House of Commons, and its current status within the House of Lords.
This timeline helps illustrate how far the bill has progressed, but also highlights that it is not yet law.
Legislative Progress of the Assisted Dying Bill

If enacted, the law would be implemented over approximately four years, with a projected operational date around 2029.
Overview of the Bill’s Provisions
Eligibility Criteria
- Age: 18 years or older
- Residency: Ordinarily resident in England or Wales for at least 12 months
- Registration: Registered with a GP in England or Wales
- Medical Condition: Diagnosed with a terminal illness expected to lead to death within six months
Mental Capacity: Must have the capacity to make an informed decision (Clause 3)
Procedural Steps
This process involves making formal requests, being assessed by two independent doctors, and undergoing a review and waiting period. Only after completing all these steps can the person choose to proceed with assisted dying, if they still wish to.
- Initial Discussion: Patient-initiated conversation with a registered medical practitioner (Clause 4)
- First Declaration: Written and witnessed declaration expressing the wish to end life (Clause 5)
- Medical Assessments: Independent evaluations by two doctors confirming eligibility (Clauses 7 and 8)
- Review Panel: Assessment by an Assisted Dying Review Panel to confirm compliance with legal criteria (Clause 10)
- Reflection Period: Mandatory waiting period of 14 days, reducible to 48 hours under certain conditions (Clause 11)
- Second Declaration: Confirmation of the wish to proceed, witnessed by the coordinating doctor and an independent witness (Clause 13)
- Provision of Assistance: Prescription of an approved substance for self-administration (Clause 21)
Understanding Assisted Dying vs. End-of-Life Pain Management
It is important to clarify that assisted dying is not the same as end-of-life pain management, which is already an established and compassionate part of medical care in the UK. Doctors routinely prescribe strong pain relief, such as opioids and sedatives, to ensure that those nearing the end of life do not suffer unnecessarily. This is known as palliative care, and it can sometimes have the secondary effect of potentially shortening life. However, the primary intention is always to relieve suffering, not to end life.
This distinction is crucial. No one should feel that their only option for relief from pain is through assisted dying. Modern palliative care offers robust and compassionate solutions for managing pain, breathlessness, agitation, and other distressing symptoms as life comes to a natural close.
The Right to Change Your Mind
Another key safeguard within the Assisted Dying Bill is the ability for individuals to change their mind at any time during the process. Whether this change is verbal, written, or communicated in any way they normally use, it must be respected. Importantly, for the cancellation to be valid and recorded, it needs to be appropriately witnessed or communicated to the coordinating doctor as per the safeguards outlined in the bill (Clause 14).
This means that even after the reflection period or the second declaration, a person can still decide not to proceed, and the process stops immediately. This safeguard is intended to ensure that no one feels locked into their decision if their circumstances, feelings, or support network change.
Areas of Concern Within the Bill
While the bill outlines a structured process, several clauses raise concerns regarding the protection of vulnerable individuals:
1. Assessment of Mental Capacity (Clause 3)
- Issue: The bill requires that individuals have the capacity to make an informed decision. However, it does not specify the qualifications or training required for practitioners assessing this capacity.
- Concern: Without stringent guidelines, there is a risk of inconsistent assessments, particularly for individuals with fluctuating mental states or communication difficulties.
2. Potential for Coercion (Clause 26)
- Issue: The bill criminalises coercion or pressure leading to a declaration for assisted dying.
- Concern: Detecting subtle forms of coercion, especially within familial or caregiving relationships, can be challenging. Vulnerable individuals may feel implicit pressure to opt for assisted dying to avoid being a burden.
3. Safeguards for Disabled Individuals
- Issue: The bill explicitly states that a person is not considered terminally ill solely due to a disability (Clause 2(3)(b)).
- Concern: Despite this provision, there is apprehension that societal biases and resource limitations could indirectly pressure disabled individuals towards assisted dying.
4. Lack of Mandatory Psychological Evaluation
- Issue: The bill does not mandate psychological assessments for individuals requesting assisted dying.
- Concern: Mental health conditions such as depression can influence decision-making. Without mandatory evaluations, there is a risk of overlooking treatable psychological issues.
5. Recording and Oversight Mechanisms
- Issue: The bill outlines the roles of medical practitioners and review panels but lacks detailed provisions for ongoing oversight and audit mechanisms.
- Concern: Continuous monitoring is essential to ensure compliance and to identify patterns that may indicate systemic issues or abuses.
My Medical Choice’s Commitment to Member Protection
In response to the potential enactment of the Assisted Dying Bill, My Medical Choice is proactively implementing measures to safeguard our members.
Our team has carefully reviewed the bill in detail, examining its clauses, provisions, and safeguards. In this article, we have highlighted the key stages of the bill, its potential risks, and, importantly, the specific sections that raise serious concerns, particularly regarding how it may impact vulnerable individuals.
We want our members to feel reassured that we are proactively monitoring every development and are fully prepared to update our systems and protections as needed.
Advance Decision Notice (ADN) Enhancements
- Explicit Opt-Out: Members can include a clear statement refusing participation in assisted dying under any circumstances.
- Comprehensive Documentation: Our ADN will allow members to detail their values, beliefs, and specific medical preferences, ensuring that their wishes are respected.
Education and Support
- Information Sessions: We will host webinars and provide resources to educate members about the implications of the bill and their rights.
- Personal Consultations: Our team is available for one-on-one discussions to assist members in updating their ADNs and addressing any concerns they may have.
Advocacy and Monitoring
- Legislative Tracking: We will continue to monitor the bill’s progression and any amendments, keeping members informed of significant developments.
- Policy Engagement: My Medical Choice will engage with policymakers and stakeholders to advocate for robust safeguards and the protection of vulnerable populations.
Frequently Asked Questions
Q1: Is assisted dying currently legal in the UK?
A: No. The Assisted Dying Bill is under consideration and has not yet become law.
Q2: Can I refuse assisted dying if the bill passes?
A: Yes. Through your Advance Decision Notice with My Medical Choice, you can explicitly state your refusal to participate in assisted dying.
Q3: Will medical professionals be obligated to participate in assisted dying?
A: No. Clause 23 of the bill stipulates that no medical practitioner is under any duty to participate in assisted dying.
Q4: How will My Medical Choice support me if the bill becomes law?
A: We will provide resources, updates, and personalised support to ensure your wishes are documented and respected.
References
- Terminally Ill Adults (End of Life) Bill – UK Parliament
- Full Text of the Bill – Parliamentary Publications
- Impact Assessment – UK Government
Some artwork taken and referenced directly from the UK Parliament site
Learn More About Protecting Your Medical Rights
At My Medical Choice, we believe that everyone deserves clarity, protection, and control over their medical decisions, especially when faced with complex laws like the Assisted Dying Bill. Our service helps you document your healthcare wishes clearly and legally, giving both you and your loved ones peace of mind in any medical situation.
* If you wish to share this article, please do so by using one of the icons listed below *
Just a friendly reminder that no information in this publication constitutes legal or medical advice from My Medical Choice or any of our affiliates and the contents of this document are for educational and support purposes only.